Introduction: Why Some Families Share More Than Just Snoring
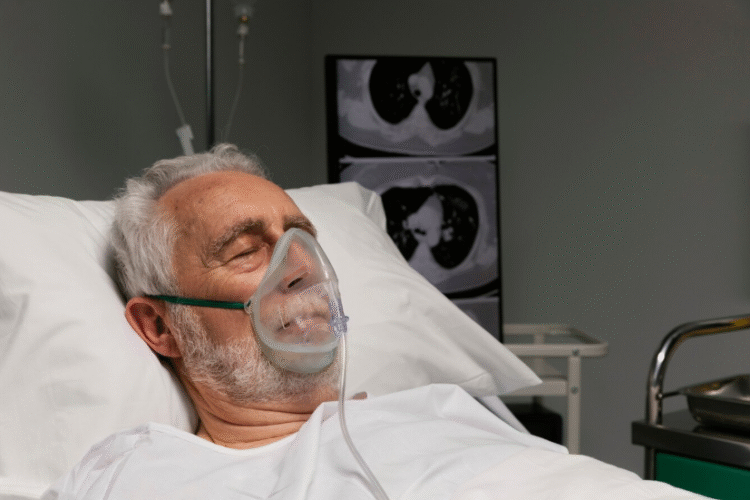
Sleep apnea has long been considered primarily a lifestyle-related condition, but groundbreaking research now reveals our DNA plays a far greater role than previously recognized. Approximately 40% of sleep apnea risk appears genetically determined, with certain families showing striking patterns of inheritance that transcend body weight or environmental factors.
This comprehensive examination explores:
- The latest genetic research on sleep apnea pathogenesis
- Key hereditary risk factors and their mechanisms
- Familial clustering patterns and inheritance models
- The promise of personalized medicine approaches
Table 1: Evidence for Genetic Contributions to Sleep Apnea
| Study Type | Key Finding | Heritability Estimate | Implications |
|---|---|---|---|
| Twin Studies | Identical twins show 73% concordance vs 38% in fraternal twins | 35-40% | Strong genetic component independent of environment |
| Family Studies | First-degree relatives have 2-4x increased risk | 30-50% | Clear familial aggregation patterns |
| GWAS Research | 97 genetic loci associated with OSA risk | 25-35% | Multiple biological pathways involved |
| Pediatric OSA | 45% of children with OSA have at least one affected parent | 40-55% | Early-onset cases show strongest genetic links |

Section 1: The Genetic Architecture of Sleep Apnea
Candidate Genes and Biological Pathways
Genome-wide association studies have identified several key genetic contributors:
Table 2: Major Genetic Loci Associated with Sleep Apnea Risk
| Gene | Chromosome | Biological Function | Risk Increase per Variant | Population Frequency |
|---|---|---|---|---|
| PDE4D | 5q12 | Airway muscle tone regulation | 18-22% | 15-20% European |
| GPR83 | 11q21 | Respiratory control signaling | 15-18% | 10-12% African |
| LEPR | 1p31 | Leptin receptor (appetite/satiety) | 25-30% | 20-25% All |
| HLA-DQB1 | 6p21 | Immune/inflammatory response | 12-15% | 30-35% Asian |
| BDNF | 11p14 | Neuronal development/maintenance | 8-10% | 40-45% All |
Inheritance Patterns and Risk Modeling
Sleep apnea demonstrates complex inheritance with multiple patterns:
- Polygenic Inheritance (Most Common)
- Combined effect of hundreds of genetic variants
- Each contributes small individual risk
- Accounts for 60-70% of genetic risk
- Mendelian Forms (Rare)
- Single gene mutations (e.g., PHOX2B in congenital central hypoventilation)
- Typically cause severe childhood-onset cases
- Account for <5% of cases
- Gene-Environment Interactions
- Genetic predisposition + environmental triggers
- Example: LEPR variants + obesity
- May explain 20-30% of cases
Table 3: Genetic Risk Stratification for Sleep Apnea
| Risk Category | Genetic Profile | Lifetime Risk | Recommended Screening |
|---|---|---|---|
| Average | <5 risk alleles | 10-15% | Routine after age 40 |
| Moderate | 5-15 risk alleles | 25-35% | Baseline sleep study by 30 |
| High | >15 risk alleles or known mutation | 50-70% | Pediatric evaluation if symptomatic |

Section 2: Mechanistic Insights – How Genes Influence Apnea Development
Craniofacial Structure Determinants
Genetic factors controlling facial development significantly impact airway anatomy:
- Mandibular Retrognathia (ABCA1, FGFR1 genes)
- Low Soft Palate (BMP4, MSX1 variants)
- Narrow Pharynx (COL2A1 mutations)
Table 4: Heritable Anatomical Risk Factors
| Feature | Heritability | Associated Genes | Clinical Impact |
|---|---|---|---|
| Maxillary Constriction | 65-70% | BMP3, RUNX2 | 3x higher AHI |
| Mandibular Hypoplasia | 60-65% | FGFR2, SOX9 | 4x higher AHI |
| Elongated Soft Palate | 55-60% | TBX22, MSX2 | 2.5x higher AHI |
| Large Tongue Base | 45-50% | GLI3, SHH | 2x higher AHI |

Neurological Control of Breathing
Genetic variants affecting respiratory drive:
- CO2 Chemosensitivity (PHOX2B, RET)
- Arousal Threshold (ADA, ADORA1)
- Upper Airway Reflexes (TRPV1, P2RX3)
Metabolic and Inflammatory Pathways
- Leptin Resistance (LEPR variants)
- Systemic Inflammation (IL6, TNFα genes)
- Oxidative Stress (SOD2, CAT polymorphisms)
Section 3: Clinical Applications and Future Directions
Genetic Testing in Sleep Medicine
Current and emerging applications:
Table 5: Genetic Testing Utility in Sleep Apnea Management
| Application | Current Status | Example | Clinical Value |
|---|---|---|---|
| Risk Prediction | Available (limited) | Polygenic risk scores | Identify high-risk individuals |
| Treatment Selection | Emerging | HLA testing for PAP adherence | Predict CPAP compliance |
| Surgical Planning | Research phase | FGFR testing for MMA outcomes | Guide surgical decisions |
| Pediatric Diagnosis | Available (targeted) | PHOX2B for central apnea | Confirm congenital forms |

Personalized Medicine Approaches
Future directions include:
- Pharmacogenomics for drug therapy selection
- Gene-targeted therapies (e.g., leptin sensitizers)
- Precision surgery based on anatomical genetics
- Preventive strategies for high-risk genotypes
Section 4: Practical Implications for Patients and Families
Family Screening Recommendations
For first-degree relatives of diagnosed patients:
- Baseline screening by age 30 (or earlier if symptomatic)
- Enhanced monitoring for metabolic comorbidities
- Preventive counseling on modifiable risk factors
Genetic Counseling Considerations
Key discussion points:
- Interpretation of complex risk information
- Implications for other family members
- Limitations of current testing
- Psychological impact of genetic risk knowledge

Conclusion: The Dawn of Genetic Sleep Medicine
The evolving understanding of sleep apnea genetics is transforming our approach to:
- Risk Prediction – Identifying susceptible individuals earlier
- Pathophysiology – Revealing novel biological mechanisms
- Treatment – Developing targeted therapies
- Prevention – Implementing genotype-specific strategies
As genetic testing becomes more sophisticated and accessible, we stand at the threshold of truly personalized care for sleep apnea patients and their families.
Call to Action:
If you have:
✓ A family history of sleep apnea
✓ Unexplained sleep symptoms despite healthy lifestyle
✓ Children with sleep or breathing concerns
Consider discussing genetic risk assessment with a sleep specialist or genetic counselor.
Additional Resources:
- National Society of Genetic Counselors: nsgc.org
- Sleep Apnea Genetics Consortium: sleepgenetics.org
- American Board of Genetic Counseling: abgc.net


0 Comments